4 May 2020 – “The road to the mountain village was rough. It’s only 50 kilometers, but it took more than 3 hours,” says Dr. Fatima Ismail, a disease surveillance officer working in Somaliland. “We were bouncing in the car.”
In early 2020, Dr. Fatima’s team headed to a remote village near Djibouti to check on a small boy. The boy’s right arm and leg showed a kind of paralysis that sometimes indicates polio. “The village polio volunteer in this mountainous area, geographically inaccessible, found an acute flaccid paralysis (AFP) case,” Dr. Fatima remembers.
When children show signs of this paralysis, it’s critical to get stool samples to a laboratory to determine whether they have polio. Polio teams ride camels in the desert or donkeys in the mountains when they have to. They brave bombs to get samples out of conflict zones to laboratories. In brutally hot climates, they plug mini-freezers into car dashboards to keep samples cool.
All over the world, polio surveillance systems that have been built up over decades track infection sources, evaluate symptoms and transport samples to the laboratory — despite the distance, natural disasters, and sometimes war. Now, this network of disease surveillance — reaching into the most far-flung corners of the globe — is being tapped to address the COVID-19 pandemic.
“In Somalia, the polio program pivoted its workforce of thousands of frontline staff to support the effort as the cases of COVID-19 spread. Rapid response teams — made up of disease surveillance officers, community health care workers, and volunteers — were trained to educate people about the virus and to test suspected cases. By April 2020, the teams were deployed in the field,” said Dr. Mamunur Malik, WHO Representative in Somalia.
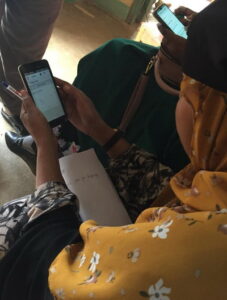
“In Somalia’s remote villages, they know us as their polio teams, and once they see us, what comes to their minds is that we’re giving them information about polio,” says Mohamed*, a surveillance officer. “So we also give them information about COVID-19. Social mobilizers tell them about COVID-19 symptoms, how to prevent getting infected, physical distancing, cleaning their hands very well with running water and soap.”
The careful procedures that the teams learned for polio surveillance have been adapted for COVID-19, where the required sample is a nasopharyngeal swab. “We’ve trained our surveillance people on the case definition and how to collect the samples correctly, from cases that meet the case definition of a suspected case of COVID-19,” says Dr. Fatima. “It’s the same infrastructure. After, when we collect the samples from the patient, we send it to the laboratory in Hargeisa.”WHO has given the laboratory equipment and supplies to test samples for COVID-19”.
“As with polio samples, the samples of COVID-19 have to be refrigerated, the ice packs should be VERY cold,” says Mohamed. Teams are used to monitoring the packs’ temperature, even in Somalia’s hot weather.
“The logistical challenges we face with AFP/polio surveillance are still the same. This is the rainy season and the roads tend to be terrible,” says Mohamed. “You can’t get to certain places you normally get to, because of the situation on the road. Most of our vehicles can’t make it through the mud.” In those situations, teams work with other United Nations agencies to arrange special humanitarian flights to ship samples.
Frontline staff put their own lives on the line. In April 2020, the polio team lost a colleague due to COVID-19-related infection. Ibrahim Elmi Mohamed, who joined WHO in 2001, was working as a district polio officer in Lower Shabelle. His tragic death, one of many frontline staff around the world due to COVID-19, reminds us of the risks they face every day they go to work.
“Despite overwhelming challenges, teams are committed to continuing their polio work in tandem with the COVID-19 response. It is critical that polio surveillance continues during the pandemic, as Somalia is also fighting outbreaks of vaccine-derived polio type 2 and 3. With polio vaccination campaigns temporarily paused, the teams must be able to track any resulting spread of poliovirus and get ready to respond as soon as it is safe to do so,” says Dr. Malik.
“All of us are still doing polio surveillance at the same time as we do surveillance for COVID-19,” says Dr. Fatima. “I used to hear from my colleagues that the polio surveillance system is the strongest disease surveillance system. Any polio surveillance team can work in the detection of COVID-19 cases because of the system’s structure, the capacity, and experience of the teams.”
Mohamed agrees. “My surveillance coordinator said don’t leave the AFP surveillance behind, follow that normal routine, don’t forget it and leave it aside.’”
As Somalia grapples with the COVID-19 pandemic, its trained teams are working quickly to prevent the spread of both COVID-19 and polioviruses. “What gives me hope in the COVID-19 response is when I look behind and I see what we have done with the polio teams, the impact we’ve had on so many lives,” says Mohamed. “We face everything and we overcome it.”
*Family name withheld for security reasons


